I. The Crisis in Your Calves: Chronic Leg Pain as a Ticking Cardiovascular Bomb atypical heart attack symptoms kolkata
A. The Deceptive Silence of Peripheral Artery Disease (PAD)
Chronic leg pain—often characterized by aching, fatigue, or cramping known medically as claudication—is an alarm bell that is frequently silenced by patient inertia and, critically, by general medical practitioners. It is common for individuals, particularly those in older age groups, to dismiss these symptoms as merely a routine component of the aging process or minor orthopedic issues. This persistent dismissal, however, allows a silent and deadly cardiovascular condition to advance undetected: Peripheral Artery Disease (PAD). atypical heart attack symptoms kolkata
PAD is far more than just discomfort in the legs; it is a profound failure of the body’s circulation system, specifically the narrowing or blockage of arteries supplying blood to the lower extremities, usually caused by atherosclerosis—the buildup of fatty plaque inside vessel walls. The failure to recognize these early warning signs has contributed to an escalating global health crisis. Data from the Global Burden of Disease study reveals that global cases of PAD surged dramatically, climbing from approximately 66 million in 1990 to more than 113 million in 2019. This massive and growing prevalence underscores the urgency required in diagnosis and intervention.
The most critical factor overlooked when chronic leg pain is generalized is that PAD is universally classified by medical guidelines as a major cardiovascular disease, not merely a localized limb problem. The pathological process of atherosclerosis that restricts blood flow in the legs often affects the coronary and carotid arteries simultaneously. Large-scale studies conclusively demonstrate that individuals diagnosed with PAD have a significantly higher concomitant risk of experiencing a heart attack or stroke. This understanding reveals a vital clinical principle: chronic leg pain is the visible sign of a hidden, deadly, systemic disease. A patient who perceives only localized discomfort is failing to address a systemic cardiovascular time bomb. Therefore, the failure to screen aggressively for PAD in high-risk patients equates to a failure to screen for imminent cardiac disaster, dramatically escalating the threat level and mandating urgent consultation with a specialist. atypical heart attack symptoms kolkata
B. Understanding the Spectrum of PAD Progression atypical heart attack symptoms kolkata
The disease pathway of PAD is characterized by distinct stages, ranging from mild states, which may be asymptomatic or only cause claudication, to the most severe and limb-threatening forms. The most critical manifestation is Critical Limb Ischemia (CLI). CLI represents the terminal stage of PAD where blood flow is so severely restricted that the tissues cannot receive adequate oxygen and nutrients. In this state, devastating complications such as non-healing ulcers, severe infections, or gangrene can develop, placing the limb in immediate and high peril of amputation.
The progression from mild claudication to severe CLI highlights why early, specialist intervention is paramount. Timely diagnosis and the initiation of targeted treatment are absolutely crucial for halting the progression of the disease and preventing these long-term, irreversible complications. The goal of specialist care is to restore robust circulation well before the patient reaches the point of ischemic crisis, securing both limb health and overall cardiovascular prognosis.
II. The Misdiagnosis Trap: The Failure of General Care and the Amputation Catastrophe atypical heart attack symptoms kolkata
A. The Cost of Missed or Delayed Diagnosis
One of the most insidious dangers of PAD lies in its high rate of misdiagnosis or delayed recognition. Because the symptoms overlap with more common, less threatening conditions, many patients are often only correctly diagnosed after the disease has already progressed significantly. General practitioners frequently miss the connection between established underlying conditions—such as existing heart disease or chronic high blood pressure—and the subsequent development of PAD. This failure in detection places the patient on a path toward devastating outcomes.
The quantitative consequence of delayed or inconsistent care is staggering. Research tracking PAD patients highlights a critical link between the continuity of care and the risk of limb loss. Patients who experienced inconsistent access to necessary, high-quality vascular care, or who suffered delays in follow-up and intervention, were found to be significantly more likely to undergo catastrophic procedures. Specifically, these patients were nearly three times more likely to require a major amputation (Odds Ratio 2.96, 95% CI 2.51–3.50) and substantially more likely to require a minor amputation (Odds Ratio 2.48, 95% CI 2.29–2.65) compared to those receiving continuous care. This stark numerical increase in risk underscores the critical reality: the longer optimal, specialized intervention is delayed, the higher the mathematical certainty of limb loss becomes.
B. The Scale of the Amputation Epidemic atypical heart attack symptoms kolkata atypical heart attack symptoms kolkata
The clinical reality surrounding PAD is that amputation is not an unavoidable fate of the disease but, in many cases, a direct consequence of suboptimal care and systemic failure to implement evidence-based diagnostics and treatment protocols. PAD has earned the grim title of the “silent amputator” because it is the single largest cause of non-traumatic amputations. In the United States alone, PAD affects over 10 million individuals and contributes to approximately 400 amputations every single day. This translates to an alarming total of around 150,000 non-traumatic leg amputations annually.
What makes this epidemic particularly unacceptable is that a substantial proportion of these amputations are potentially preventable. Despite the existence of clear, evidence-based diagnostic and therapeutic approaches that can significantly reduce amputation risk, the implementation and patient adherence to these strategies remain suboptimal. This failure is most acutely observed in the highest-risk group: patients with diabetes, who account for the majority of non-traumatic amputations. Following a period of decline, amputation rates among diabetic patients shockingly increased by 50% between 2009 and 2015. This resurgence proves that general practice is often failing to deliver the optimal, life- and limb-saving management that is required. Therefore, the excessively high rate of amputation reflects a failure of implementation and care continuity, establishing that specialized, proactive intervention is urgently needed to interrupt this dangerous trend.
III. Your Personalized Warning: Mapping the High-Risk Profile atypical heart attack symptoms kolkata
Identifying and acting on high-risk factors is the essential first step in limb preservation. For individuals with chronic leg pain, recognizing specific co-morbidities transforms the general health warning into a highly relevant, urgent personal appeal.
A. The Acute Risk for the Diabetic Population
The link between Type 2 Diabetes Mellitus (T2DM) and PAD is profound, particularly within the target demographic. A recent systematic review and meta-analysis focusing on the Indian population confirmed that the combined prevalence of PAD among individuals with T2DM is a significant 18%. This means that nearly one in five diabetic patients in the region is affected by this circulatory crisis, justifying the immediate need for specialist consultation and diagnostic testing.
When assessed across various high-risk patient cohorts—including those with Ischemic Stroke (IS), Cardiovascular Disease (CVD), or Diabetes Mellitus (DM)—the overall prevalence of PAD detected by the Ankle-Brachial Index (ABI) was found to be 27.1%, with the prevalence being highest specifically among those with DM. Age and the duration of DM were consistent risk factors across all cohorts. Furthermore, demographic analysis indicates that the risk profile for this patient population is highly specific: for South Asians, diabetes, smoking, male sex, and mean systolic blood pressure were all independently associated with PAD. By understanding the elevated 18% prevalence among T2DM patients in the region , the post moves beyond being a general advisory and becomes a direct, hyper-relevant call to action, establishing the high likelihood of disease and justifying immediate specialized assessment.
B. The Pervasive Threat of Hypertension
Beyond diabetes, high blood pressure (hypertension) is recognized as a major independent force driving the arterial damage that precedes and exacerbates PAD. The causal mechanism is clear: high BP damages the delicate lining of the artery walls, accelerates the atherosclerotic process, and increases arterial stiffness. A landmark study in the Atherosclerosis Risk in Communities (ARIC) cohort found that people with hypertension had a 1.5 to 2 times higher risk of developing PAD compared to those with normal blood pressure levels. This data confirms that for patients managing hypertension, leg pain should never be dismissed; it is a signal that the ongoing arterial damage has reached the periphery.
C. The Imperative of Specialized Screening
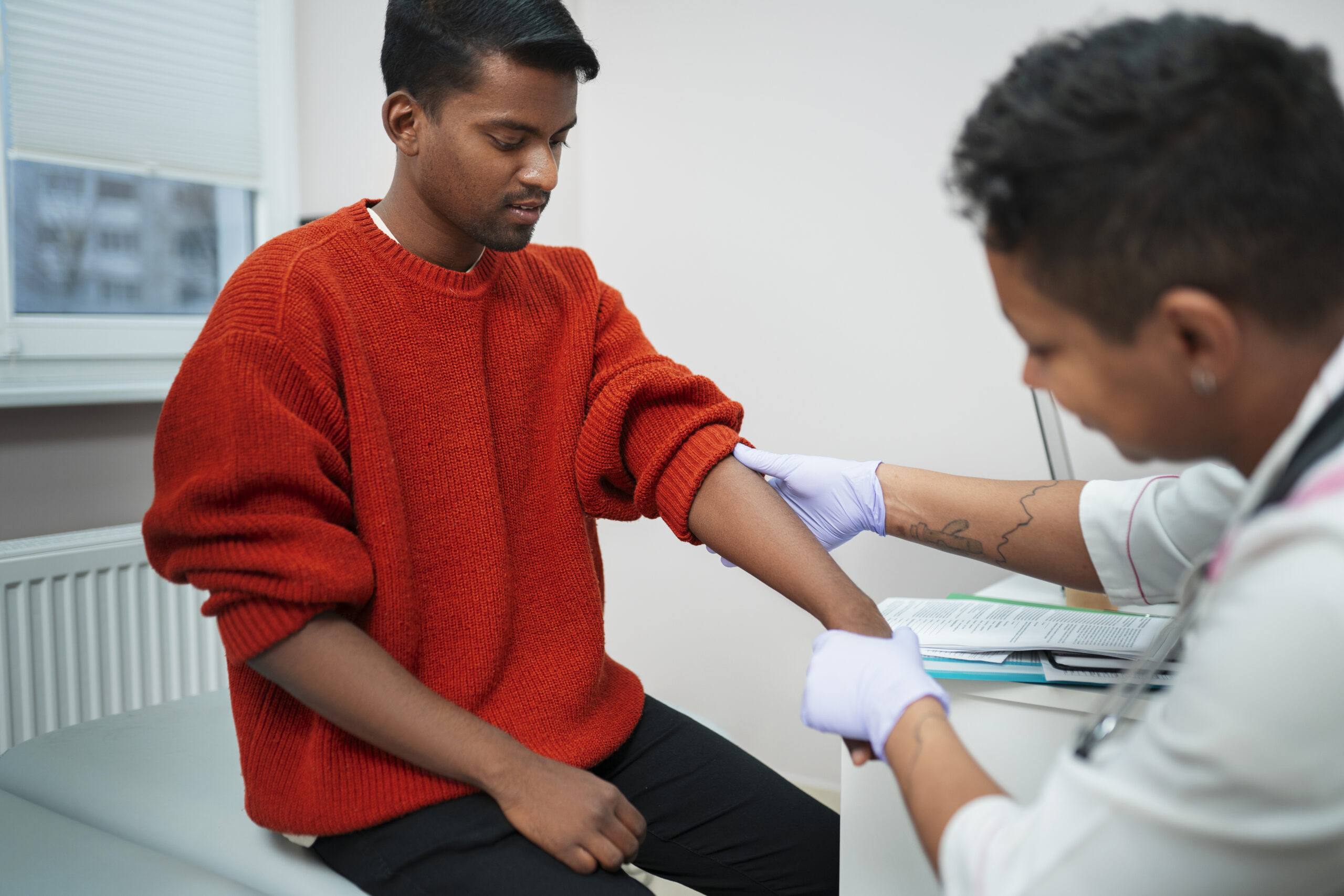
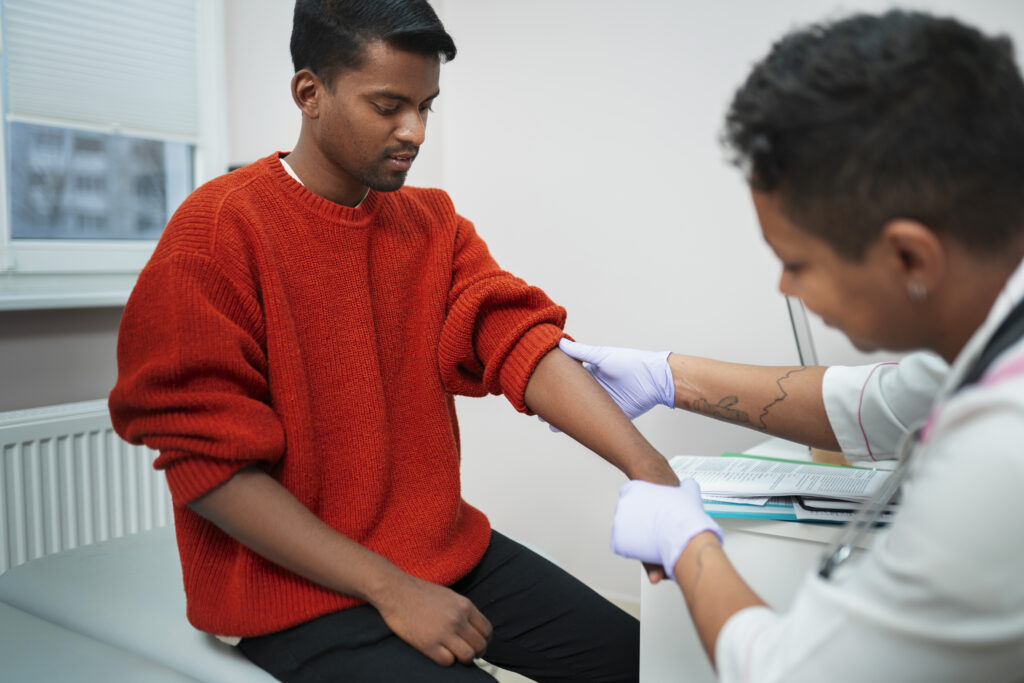
Given the high prevalence and severe consequences, current medical consensus globally mandates specialized screening for PAD in high-risk groups. Specifically, screening using the Ankle-Brachial Index (ABI)—a non-invasive assessment comparing blood pressure in the ankle to the arm—should be routinely performed among patients with ischaemic stroke, cardiovascular disease, or diabetes mellitus.
For a patient reading this and recognizing their own risk factors (T2DM, hypertension, smoking history, or chronic leg pain), the critical question becomes: has my general practitioner performed this essential, life-saving screening? If the answer is no, the patient is almost certainly receiving suboptimal care. The specialist’s role begins precisely here—by moving beyond generalized assumptions of “old age” and providing the targeted, evidence-based vascular screening required to catch the disease before it leads to critical limb ischemia or amputation.
IV. The Pivot to Limb Preservation: Why Endovascular Treatment is Statistically Superior atypical heart attack symptoms kolkata
For patients facing chronic PAD, the choice of intervention is crucial, often representing the decisive factor between limb preservation and amputation. Advanced peripheral intervention specialists focus on techniques that are not merely minimally invasive, but maximally successful for long-term survival and limb salvage.
A. The Endovascular Advantage: Risk Reduction and Recovery
Dr. Avishek Saha specializes in advanced endovascular procedures—techniques performed through small vessel punctures to restore arterial blood flow (revascularization) with minimal patient trauma. This approach is scientifically substantiated to provide superior outcomes compared to traditional, highly invasive open surgical bypass.
Clinical studies demonstrate that an endovascular procedure is associated with a risk-adjusted 16% decreased risk of amputation or death when compared to open revascularization over the study period. This single data point—a 16% improvement in the combined metric of life and limb preservation—is the ultimate validation of the specialized approach. It confirms that endovascular care is not just about avoiding large incisions; it directly translates to improved life and limb survival rates. Beyond the mortality benefit, endovascular surgery provides significant advantages in terms of complication profile and recovery dynamics. It results in fewer complications, shorter hospital stays, and a lower overall mortality rate when compared with traditional open surgery, even while achieving similar rates of technical success and limb salvage.
B. Amplified Benefit for Complex Cases
The benefits of the endovascular approach are particularly pronounced where the patient risk is highest. The amputation-free survival benefit associated with endovascular revascularization was found to be significantly more pronounced in patients with complex co-morbidities, such as congestive heart failure (CHF) or ischemic heart disease (IHD), than in those without these conditions. This suggests that the specialized, less traumatic nature of endovascular techniques provides essential protection for patients whose systemic health status might make them poor candidates for major open surgery.
Furthermore, for the most severely affected patients—those who have already progressed to Critical Limb Ischemia (CLI)—the amputation-free survival benefit associated with an endovascular approach persisted, proving its efficacy precisely at the point of greatest danger. While endovascular procedures may sometimes require more vigilant, ongoing maintenance (with a slightly higher rate of subsequent intervention compared to open surgery—7.4% greater at 30 days) , this reflects a paradigm of proactive, sustained disease management rather than relying on a single, high-risk, potentially devastating surgical intervention.
C. Comparative Treatment Outcomes
The clinical evidence overwhelmingly favors the specialized endovascular approach for limb preservation and improved short-term safety profiles. The following comparative data synthesized from major clinical studies underscores the difference between traditional and modern intervention strategies.
Superior Outcomes: Endovascular Intervention vs. Open Surgery
| Metric | Specialized Endovascular Intervention | Traditional Open Surgery (Bypass) | Impact on Patient Outcome |
| Risk of Amputation or Death | 16% Decreased Risk (Risk-Adjusted) | Higher Baseline Risk | Maximally successful for life and limb preservation. |
| Complication Rate | Lower | Higher | Reduces post-operative morbidity and risk. |
| Hospital Stay | Shorter Duration | Longer, More Invasive Stay | Faster recovery and reduced risk exposure. |
| Early Mortality Rate (30-day) | Diminished Mortality (5.3% rate) | Higher Mortality (6.7% rate) | Demonstrates a superior safety profile in the immediate post-procedure critical window. |
V. Meet the Specialist: Dr. Avishek Saha’s Comprehensive Toolkit for Advanced PAD
A patient seeking limb preservation requires assurance that their chosen physician is equipped not just for standard procedures, but for the complex, calcified, and potentially failed previous interventions that define advanced PAD. Dr. Avishek Saha’s practice focuses on utilizing the full arsenal of contemporary endovascular technology, ensuring preparedness for the most challenging arterial blockages.
A. Expertise in Complex Revascularization Techniques
Specialized peripheral intervention moves beyond conventional ballooning to address complex lesions, particularly Chronic Total Occlusions (CTO)—arteries that have been 100% blocked for an extended duration. Treating CTOs requires immense skill and specialized strategies, such as subintimal dissection and true lumen re-entry, which are frequently employed in complex revascularization scenarios. The presence of these highly technical skills signals an ability to manage cases often deemed “untreatable” by non-specialists.
The advanced services provided encompass a comprehensive range of state-of-the-art tools necessary for high technical and procedural success rates, even in the most difficult clinical scenarios. These advanced devices and treatments include:
- Atherectomy: Mechanical removal of hard plaque buildup to prepare the vessel for ballooning and stenting. Although often used, registry data suggests careful selection for this approach.
- Specialized Balloons: This includes conventional angioplasty (PTA), as well as Drug-Coated Balloons (DCB), which deliver medication directly to the vessel wall to prevent re-narrowing, and scoring or cutting balloons to facilitate opening rigid lesions.
- Stenting Options: Both Drug-Eluting Stents (DES), which offer medication release to reduce recurrence, and standard Bare-Metal Stents (BMS) are utilized strategically, based on lesion morphology.
High technical and procedural success rates are achievable through the frequent and strategic use of these combination treatments. The ability to deploy atherectomy, specialized balloons, and navigate CTOs confirms the practice’s focus on limb salvage, reassuring patients—especially those with severe blockages—that they are consulting an expert prepared for the most intricate cases.
B. The Difference Between a Generalist and a Peripheral Intervention Expert
The difference between a generalist (like a primary care physician or sometimes a general cardiologist) and a specialized peripheral intervention expert is one of strategic focus. While a generalist focuses on risk factor management (medication, lifestyle changes), a peripheral intervention specialist, such as Dr. Saha, focuses acutely on restoring flow, preserving tissue, and achieving limb salvage.
The utilization of a vast and complex toolkit—including atherectomy, DCB, and techniques to manage severe CTOs—is the definitive evidence of specialized capability. It shows that the expert is capable of achieving revascularization in cases where generalized treatment may have plateaued or where a patient has received a poor prognosis elsewhere. Given that suboptimal implementation of existing evidence-based approaches contributes directly to the rising trend of non-traumatic amputations , seeking out a practitioner who consistently employs these advanced, successful strategies is the critical step toward avoiding irreversible damage. atypical heart attack symptoms kolkata
VI. Urgent Call to Action: Take Control Before the Damage is Done atypical heart attack symptoms kolkata
A. The Deadline: Why You Cannot Afford to Wait
The data presented here is not an academic discussion; it is a clinical warning. The stark fact that delayed intervention can increase the risk of a major amputation by nearly three times (Odds Ratio 2.96) should be treated as a definitive clinical deadline. Every day chronic leg pain is dismissed as “routine aging” is a day the underlying atherosclerotic plaque continues to build, pushing the patient closer to irreversible Critical Limb Ischemia (CLI). atypical heart attack symptoms kolkata
This immediate urgency aligns with broader public health objectives. Leading medical organizations, including the American Heart Association (AHA), have issued urgent calls for actionable policies to enhance the delivery of optimal PAD care with the goal of reducing non-traumatic lower-extremity amputations by 20% by 2030. A patient’s decision to immediately seek specialized assessment and intervention is a direct participation in this vital, limb-saving movement.
B. Secure Your Limb, Secure Your Future: Next Steps for Specialized Assessment atypical heart attack symptoms kolkata
If an individual experiences persistent chronic leg pain, cramping, non-healing sores, or if they possess known high-risk factors such as a history of diabetes (where PAD prevalence approaches 18% in the regional demographic ), high blood pressure, or established cardiovascular disease, an immediate specialized vascular assessment is mandatory. atypical heart attack symptoms kolkata
The most critical initial step is a comprehensive Peripheral Vascular Assessment, which must include routine Ankle-Brachial Index (ABI) screening, conducted and expertly interpreted by a peripheral intervention specialist. It is imperative that patients do not rely solely on a general diagnosis that fails to recognize the severity of systemic cardiovascular disease manifesting in the legs. Only specialized expertise designed explicitly for limb preservation and advanced revascularization can interrupt the dangerous pathway leading to amputation. atypical heart attack symptoms kolkata
C. Contact Dr. Avishek Saha Today
The path to proactive limb preservation and cardiovascular safety starts with one urgent, decisive action. Do not wait for symptoms to progress to the point of irreversible tissue damage or the threat of amputation.
Dr. Avishek Saha Healthcare Contact Number: +91 9874381872 Website: www.dravisheksaha.com
Conclusion and Recommendations atypical heart attack symptoms kolkata
The evidence overwhelmingly establishes Peripheral Artery Disease as a widespread, escalating cardiovascular threat whose most devastating consequence, non-traumatic amputation, is often a direct result of delayed diagnosis and suboptimal care implementation. The high prevalence among regional high-risk groups, particularly diabetic patients, necessitates immediate and targeted screening.
The specialized approach of endovascular intervention, as practiced by experts like Dr. Saha, offers a statistically superior pathway for limb and life preservation, providing a risk-adjusted 16% reduction in amputation or death compared to traditional methods. The demonstrated capability to manage complex lesions, including CTOs and heavy use of advanced devices like atherectomy, confirms the practice’s focus on maximizing flow restoration where general treatment has failed. For any individual experiencing chronic leg pain or possessing known PAD risk factors, the recommended action is immediate consultation to leverage specialized diagnostics (ABI) and access advanced endovascular therapies before the disease progresses to critical, irreversible stages where the risk of major amputation increases nearly threefold.